Sports & Play SAFETY
Concussion Prevention
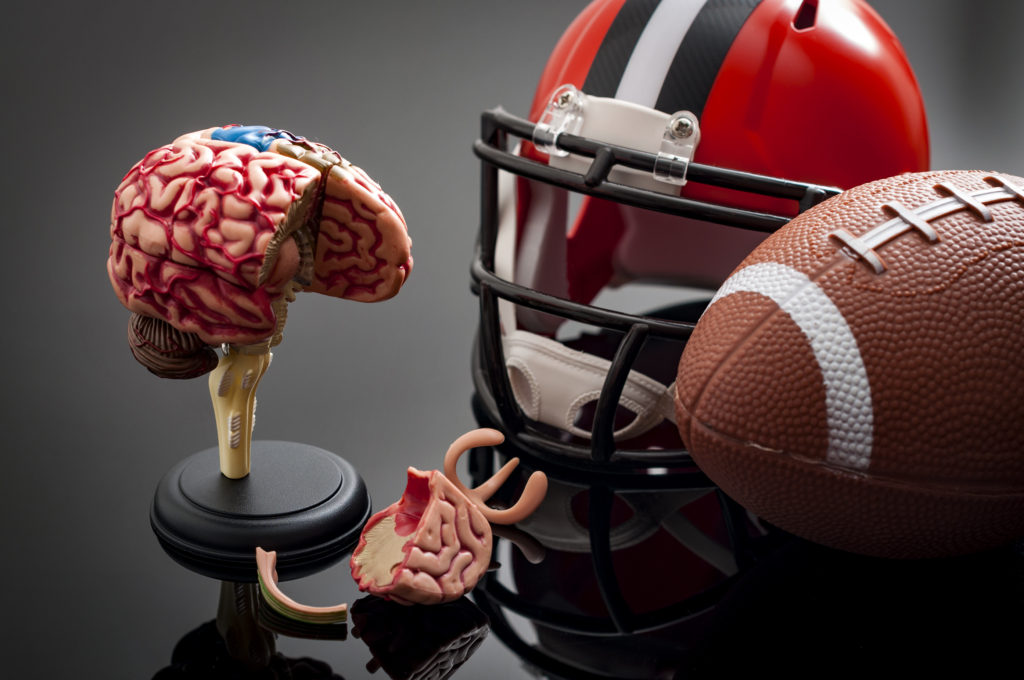 A concussion is a type of traumatic brain injury (TBI) caused by a bump, blow, or jolt to the head or by a hit to the body that causes the head and brain to move rapidly back and forth. The sudden movement can cause the brain to bounce around the skill, creating chemical changes in the brain and sometimes stretching or damaging brain cells. All concussions are serious and anyone with a suspected concussion needs to see a health care professional as soon as possible.
A concussion is a type of traumatic brain injury (TBI) caused by a bump, blow, or jolt to the head or by a hit to the body that causes the head and brain to move rapidly back and forth. The sudden movement can cause the brain to bounce around the skill, creating chemical changes in the brain and sometimes stretching or damaging brain cells. All concussions are serious and anyone with a suspected concussion needs to see a health care professional as soon as possible.
Safety Tips
General Tips (Non-Sports)
- Always use age- and size-appropriate car seats and booster seats that are properly installed.
- Make sure your child always wears the right helmet for their activity and that it fits correctly. Wearing a helmet is a must to help reduce the risk of a serious brain injury or skull fracture. However, helmets are not designed to prevent concussions. There is no “concussion-proof” helmet.
- Use gates at the top and bottom of stairs to prevent serious falls in infants and toddlers.
- Use playgrounds with soft material under them like mulch or sand, not grass or dirt.
- If a child has a concussion, make sure to follow all medical advice until the child is fully healed (a process which could take a few weeks to months).
Sports-Specific Tips
- Create a safe sports culture.
- Enforce the rules of the sport for fair play, safety, and sportsmanship and make these expectations clear. Ensure that athletes avoid unsafe actions such as striking another athlete in the head, making illegal contacts or checking, tackling, or colliding with an unprotected opponent, and/or trying to injure or putting another athlete at risk for injury. If athletes engage in these unsafe behaviors, do not let the continue playing in the game.
- Talk about concussion reporting and the importance of reporting it. Make sure that athletes understand how serious concussions are, and the potential long-term impacts of untreated concussions as well as repeated concussions.
- Create a concussion action plan. If you think an athlete may have a concussion, you should:
- Remove the athlete from play.
- Keep that athlete out of play on the same day of the injury and until they are cleared by a health care provider. Do not try to judge the severity of the injury yourself. Rely on the expertise of a health care provider for the assessment.
- Record and share information about the injury (such as how it happened and the athlete’s symptoms) in order to help a health care provider’s assessment.
- Inform the athlete’s adult caregiver(s) about the possible concussion and include steps that they should take next.
- Ask for written instructions from the athlete’s health care provider about the steps you should take to help the athlete safely return to play.
- Before returning to play, an athlete should be back to doing their regular school activities, not have any symptoms from the injury when doing normal activities, and have the green-light from their health care provider to begin the return to play process.
- If helmets are required in the sport, make sure the athlete is wearing a helmet that is the correct size and fit, and is in good condition.
- Work with the game or event administrator to remove tripping hazards and ensure that equipment has padding that is in good condition.
- Teach athletes proper techniques and ways to avoid hits to the head.
- Limit the amount of contact in sports practices.
- Keep a close eye on athletes in positions that are at increased risk for concussion to help you spot a potential concussion.
- For Cheerleading: make sure that cheerleaders have appropriate supervision during practices as well as a designated and safe practice facility. Limit the amount of stunts during practices, and always use spotters when stunting. Teach safe stunting techniques and do not allow any new or difficult stunts without proper instruction and a coach present.
Signs and Symptoms
Observed Signs and Symptoms include:
- Appears dazed or stunned
- Is confused about assignment or position
- Forgets sports plays
- Is unsure of game, score, or opponent
- Moves clumsily
- Answers questions slowly
- Loses consciousness (even briefly)
- Shows behavior or personality changes
- Cannot recall events prior to hit or fall, and/or cannot recall events after hit or fall.
Reported Signs and Symptoms include:
- Headache or “pressure” in the head
- Nausea or vomiting
- Balance problems or dizziness
- Double or blurry vision
- Sensitivity to light
- Sensitivity to noise
- Feeling sluggish, hazy, foggy, or groggy
- Concentration or memory problems
- Confusion
- Does not “feel right.”
Severe Signs and Symptoms include:
- One pupil is larger than the other.
- Drowsiness or inability to wake up.
- A headache that gets worse and does not go away.
- Slurred speech, weakness, numbness, or decreased coordination.
- Repeated vomiting or nausea, convulsions or seizures (shaking or twitching).
- Unusual behavior, increased confusion, restlessness, or agitation.
- Loss of consciousness (passed out/knocked out). Even a brief loss of consciousness should be taken seriously.
- For infants or toddlers, any of the above signs OR
- Will not stop crying and cannot be consoled.
- Will not nurse or eat
Call 9-1-1 right away, or take your child or teen to the emergency department if they have one or more of the above danger signs after a bump, blow, or jolt to the head or body.
Steps to Take When a Concussion is Suspected
- Seek medical attention right away – A health care professional will be able to decide how serious the concussion is and when it is safe for your child to return to activities.
- Keep your child out of play – Concussions take time to heal. Do not let your child return to play until cleared by a health professional. Returning to play before healing can prolong symptoms and increase the risk of another concussion.
- Tell your child’s coach about any recent concussion – Coaches should know if your child had a recent concussion.